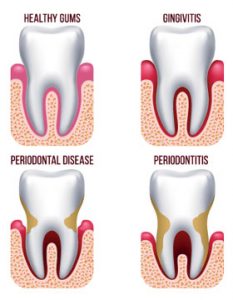
Gum disease is an inflammation of the gum that can progress to affect the bone that surrounds and supports your teeth. The three stages of gum disease — from least to most severe — are gingivitis, periodontitis and advanced periodontitis.
Signs and Symptoms
Gum disease can be painless, so it is important to be aware of any of the following symptoms:
- Gums that bleed easily when brushing or flossing
- Swollen, red or tender gums
- Gums that recede or move away from the tooth
- Persistent bad breath or bad taste in your mouth
- Loose teeth
- A change in the way your teeth come together
- A change in the fit of partial dentures
- Visible pus around the teeth and gums
Diagnosis
The Bacteria in plaque, a sticky, white film that constantly forms on your teeth, cause gum disease. If plaque is not removed it can harden and turn into tartar (calculus). Additionally, dental plaque will continue to form on the tartar. Brushing or flossing cannot remove tartar; a dental practitioner will need to conduct a dental cleaning to remove it. If not removed through daily brushing and flossing, plaque turns into tartar, which becomes a rough and retentive surface encouraging further buildup of plaque. The plaque bacteria can cause gum inflammation and eventually, the gum tissue and the bone that support the teeth can be affected. There are three stages of gum disease:
Gingivitis – This is the earliest stage of gum disease. It is the inflammation of the gums, caused by dental plaque buildup at the gum line. You may notice some redness or swelling of the gums, or some bleeding during brushing and flossing. At this early stage gum disease can be reversed since the bone and connective tissue that hold the teeth in place are not yet affected.
Periodontitis – At this stage, the supporting bone and fibers that hold the teeth in place are irreversibly damaged. A pocket below the gum line forms, which encourages growth of plaque in this area. Professional periodontal therapy and improved personal oral hygiene can usually help prevent further damage to the gum tissue supporting tissue and bone.
Advanced Periodontitis – In this more advanced stage of gum disease, the fibers and bone that support your teeth have largely been destroyed, which can cause your teeth to shift or loosen. This can affect your bite and how you eat and communicate. If aggressive periodontal therapy can’t save them, teeth may need to be removed by a dentist. Your dentist will also provide restorative options if teeth are removed due to periodontal disease.
Treatment

A professional cleaning by your dental practitioner is the only way to remove plaque that has built up and hardened into tartar. By scheduling regular checkups — twice a year — early stage gum disease can be treated before it leads to a much more serious condition.
If gum disease is more advanced, scaling and root planning can be performed to treat diseased periodontal pockets and gum infection Dental practitioners may use an ultrasonic scaling device to remove plaque, tartar and food debris above and below the gum line, and hand scalers on the tooth and root surfaces to make them smooth. Quite often our patients with periodontal disease will see our dental health therapist every few months to have the cleaning process repeated.
Occasionally patients with gum disease may need to have their clean broken up into four appointments. This means our oral health therapist can concentrate on one quadrant of your mouth each visit. You may be given a local anaesthetic to ensure you are comfortable throughout the cleaning treatment.
If periodontal pockets are more than 5 millimetres deep, that is, if you have moderate to severe periodontitis, gingival flap surgery may be performed by a periodontist to reduce periodontal pockets, remove deposits from root surfaces, and perhaps provide bone grafting to restore lost bone.